Version 7, October 28, 2018

A few years ago I was at my yearly appointment with my endocrinologist, when she asked me, “Beverly, I wish I could convince more of my new patients to start out on injections. Too many of them just want pills. Do you have any suggestions?” I think I said something about needle and syringe selection, so that patients were not being forced to use 22 gauge needles — or some other unhelpful comment. But I knew that really wasn’t enough — something easier, and less scary, was badly needed. Shortly after, I learned of a patient in Canada using estradiol valerate (EV) subcutaneous injections, and decided to try it on myself. After a few months of experiments and tests I was ready to mention it to others, and after finding a medical study verifying its effectiveness, I was ready to recommend it to doctors too — many of whom, it turns out, were already quietly using it on their patients.
I’ll begin with practical information. Following that will be the medical and clinical information, experimental results, and group knowledge.
To start, you need to get the right syringe and needle combination. Pharmacists, nurses, and most doctors have not been trained on best practice for oily hormones by subcutaneous methods, and usually recommend the wrong equipment — equipment suitable for vaccinations, antibiotics, insulin, etc. Oil based hormones have different requirements. If you doubt that, ask a doctor specializing in fertility treatments.
 Getting the right equipment requires first determining the volume of hormones per injection. For best results it must be less than 1cc (which equals 1 milliliter, or 1 ml.) so that a small diameter syringe can be used, which enables use of a 30 gauge needle with high viscosity liquids. (Due to the laws of hydraulics.) If you inject 2ml of hormones per 10 days, for instance, you will need to split it and change your schedule to 1ml every 5 days. (Larger syringes such as the 3ml syringe are not suitable because they make using small needles impossible with oily hormones — don’t let your pharmacist give you the wrong syringes!) This determines the type of equipment you must use. There are two cases. Check to see which applies to you.
Getting the right equipment requires first determining the volume of hormones per injection. For best results it must be less than 1cc (which equals 1 milliliter, or 1 ml.) so that a small diameter syringe can be used, which enables use of a 30 gauge needle with high viscosity liquids. (Due to the laws of hydraulics.) If you inject 2ml of hormones per 10 days, for instance, you will need to split it and change your schedule to 1ml every 5 days. (Larger syringes such as the 3ml syringe are not suitable because they make using small needles impossible with oily hormones — don’t let your pharmacist give you the wrong syringes!) This determines the type of equipment you must use. There are two cases. Check to see which applies to you.
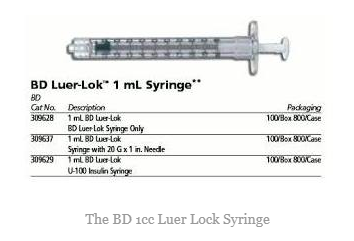
Case 1: This applies to you if each time, you inject more than 0.3cc but less than 1cc. You will need 3 things: (1) a 1cc Luer Lock syringe, (2) a draw needle, and (3) an injection needle.
For Case 1, item #1, the syringe, I suggest three alternatives. These BD syringes are excellent, at about 50 cents each: http://www.allegromedical.com/syringes-c570/syringe-luer-lok-1cc-sp-p550722.html. The Kendall syringes are quite adequate, for about 40 cents each: https://www.mdsupplies.com/medical-supplies-Kendall-SYRINGE-1cc-TB-LL-WZPRDXDUQ9.html. The Easytouch brand is not personally familiar to me, but is very low cost at under 30 cents each: https://www.missourimedicalsupplies.com/easytouch-1cc-luer-lock-syringe-bx-100/ . You will find other sources for each of the above syringes, with varying prices and availability. Note: take care that you do NOT accidentally buy the “Luer Slip” style of syringe — such syringes do not lock to the needle, but instead they slip on more loosely, inviting a “pop off” accident when injecting oily hormones. Slip-type syringes are only suitable for less viscous injections such as vaccines. Luer-Lock syringes twist on the needle, making it impossible for it to leak or pop off when injecting oily hormones, which may require more pressure. If you are in a location where ordering syringes is restricted, you can try ordering thru EBAY, which generally evades such restrictions. Here is a typical listing.
For Case 1, item #2, the draw needle, I prefer a 1.5 inch 20 gauge needle such as: https://www.mdsupplies.com/medical-supplies-Dynarex-Hypodermic-Needle-20G-1-12-needle-25CXRSY64J.html See this listing for a typical EBAY source, if you have trouble ordering from other sources.
For Case 1, item #3, use a 0.5 inch 30 gauge needle, such as this inexpensive one:
https://www.mdsupplies.com/medical-supplies-Exel-Hypodermic-Needle-30g-x-12-4GPJ5A6DRL.html See this listing for a typical EBAY source, if you have trouble ordering from other sources.
 Case 2: this applies to you if each time, you inject 0.3cc or less. For this low volume, instead of following Case 1 above, you MAY choose (it’s optional) to use the all-in-one insulin syringe. In choosing case 2, keep in mind that this has a disadvantage that filling the syringe is VERY time consuming because it has to be drawn thru a 30g needle. Also, its needle is not as sharp, and may be slightly less painless to use. If either of these factors will bother you, go back to Case 1. Otherwise, in this case, you only need to buy one piece of equipment — the 0.3cc insulin syringe. Here is one in a box of 100: http://www.allegromedical.com/syringes-c570/ultra-fine-syringe-lo-dose-p191846.html. Here is a typical EBAY source listing. And this inexpensive source. Now you’re set.
Case 2: this applies to you if each time, you inject 0.3cc or less. For this low volume, instead of following Case 1 above, you MAY choose (it’s optional) to use the all-in-one insulin syringe. In choosing case 2, keep in mind that this has a disadvantage that filling the syringe is VERY time consuming because it has to be drawn thru a 30g needle. Also, its needle is not as sharp, and may be slightly less painless to use. If either of these factors will bother you, go back to Case 1. Otherwise, in this case, you only need to buy one piece of equipment — the 0.3cc insulin syringe. Here is one in a box of 100: http://www.allegromedical.com/syringes-c570/ultra-fine-syringe-lo-dose-p191846.html. Here is a typical EBAY source listing. And this inexpensive source. Now you’re set.
INJECTION INSTRUCTIONS
Fill the syringe with the proper dose of your oil-based hormones (Estradiol Valerate, Estradiol Cypionate, Progesterone in Oil, Testosterone Cypionate/ Propionate/ Enanthate/ etc.) How you do this depends on how your hormones are packaged, and I have covered that subject elsewhere. I’ll assume you know how to fill your syringe, and have done so, and are ready to inject.
The location should be in a part of your body which has a fatty layer. Choose either your abdomen or your hip. If it is the abdomen, it must be at least 4 inches away from your navel, where the fatty layer thins. Here is the procedure, spelled out.
 (1) With the needle attached to the syringe and all air expelled, loosen the cap of the needle, then lay the syringe down within reach.
(1) With the needle attached to the syringe and all air expelled, loosen the cap of the needle, then lay the syringe down within reach.
(2) Apply alcohol to the area to be injected. LET DRY COMPLETELY. Don’t blow on it, but you can fan it with something if you are impatient. It may sting if your skin isn’t dry.
(3) Using one hand, pinch your skin between thumb and forefinger. Not too hard.
(4) With the other hand, pick up the syringe, and tilt it so that the cap falls off the needle.
(5) Then gently place the 30 gauge needle on the skin at a 45 degree angle to your skin. While gently touching the skin, you may move the tip a tiny bit to a place with the least sensation. Then while applying the lightest pressure you can, use a gentle twisting motion back and forth of the syringe, like you are spinning it slightly in your fingers. The needle will sort of swim into your skin with minimum sensation. When I do this, the sensation is often so little that I would not know it had happened if I wasn’t watching. The spinning motion seems to cause the nerves, which are sort of tough, to simply move out-of-the-way a bit as the needle moves past. Do NOT jab. Spin the needle in very lightly. Once you get familiar with this technique, you can make a game of it — see how completely painless you can make it.
(6) Now that the needle is fully inserted, you may release the pinch on your skin. Relax and use both hands to withdraw the plunger slightly to verify that you are not in a vein. (This is optional.) Then press the plunger to inject. Remove the needle. You’re done. The change in the tension on your skin, when you released the pinch, will help to prevent any leaking or a drop of blood from showing. But don’t be anxious if you see a drop of either. You’re all right. Wipe again with alcohol.
I have two videos. This one is for Case 1, using the conventional Luer Lock syringe: https://youtu.be/KooPrAWrlFA
This one is for Case 2, with the insulin syringe: https://youtu.be/kcIFYL-mDlQ
Now let’s talk about the medical aspects.
The location recommended by manufacturers for hormone injection is the buttocks (NOT the thigh!). But a recent study shows that the blood levels for fat layer subcutaneous injection (“SubCut”) of these oil-based hormones will be similar to gluteal IM.(ref 1) So, why would we consider a SubCut injection, if we are already giving ourselves a buttocks IM injection? First, one reason doctors have for refusing to allow their transsexual patients to inject themselves is fear that they might hit the Sciatic nerve. This mistake is almost unheard of when injections are done by trans women – the scare stories are nearly all of novice nurses doing this – but it’s been a pretext used by doctors to deny injection as an option to their patients. You can sidestep this objection by requesting your doctor set you up to do your hormones by SubCut instead. If your doctor objects that hormones are not specified to be administered that way by the manufacturer (which is true) you can give them this article (1) to read, which proves that the method can have similar effectiveness. Furthermore, you should present this proof that subcutaneous injection is widely used, effective, and safe for FTM trans men. (3) In both cases, the injection is an oil-based steroid ester – if one works well, the other should also. In this way, SubCut can be a bargaining tool you can use to get your doctor to start you on injections. Second, a proper IM injection into the gluteus generally requires that you be standing. Not all trans women can stand while injecting — some may be wheelchair bound, feel unconfident, or be otherwise disabled. These patients can benefit from SubCut abdomen or hip injections of hormones, which can be easily done while sitting. And finally, many patients are anxious that injections might hurt and they avoid injections, but these subcutaneous injections are so painless that few patients will object. Those who are needle phobic should find it easier to deal with the tiny needles.
 Informal testing on myself, comparing the bioavailability of hormones each way, showed that the SubCut method is at least 85% the efficiency of conventional Gluteus Medius/Maximus IM injections. The half life is slightly shorter, but similar. My informal results were confirmed by blood tests as well. In group settings, we generally observe that best feminization is observed with the shortest cycles, with a twice-a-week cycle giving a significant benefit. This fits the overall observation that best feminization is achieved more by avoiding estradiol dropouts than by creating estradiol surges. A once-a-week cycle for Estradiol Cypionate seems to be good, but Estradiol Valerate does not do as well when stretched that far. I do not have good data on testosterone esters in this respect, but any injection schedule which prevents peak/trough ratios from exceeding about 1.5 appears to give good results and I personally believe this applies to all the esters.
Informal testing on myself, comparing the bioavailability of hormones each way, showed that the SubCut method is at least 85% the efficiency of conventional Gluteus Medius/Maximus IM injections. The half life is slightly shorter, but similar. My informal results were confirmed by blood tests as well. In group settings, we generally observe that best feminization is observed with the shortest cycles, with a twice-a-week cycle giving a significant benefit. This fits the overall observation that best feminization is achieved more by avoiding estradiol dropouts than by creating estradiol surges. A once-a-week cycle for Estradiol Cypionate seems to be good, but Estradiol Valerate does not do as well when stretched that far. I do not have good data on testosterone esters in this respect, but any injection schedule which prevents peak/trough ratios from exceeding about 1.5 appears to give good results and I personally believe this applies to all the esters.
Since 2016 at the latest, all or nearly all MTF and FTM patients at The Mayo Clinic are going on Subcutaneous injection from Day 1, according to one of the patients in the program. (2) MTF patients use the 20mg/cc or 40mg/cc strength of Estradiol Valerate. Dr. Todd Nippoldt is in charge of the program. The doctor has published nothing I can find so far on MTF using subcutaneous, but given his program, I would imagine that a paper will be published soon. That would be the first, and would surely be very influential. The patient I contacted reports that everyone is doing well and that the clinic staff are talking about it in their presentations.
At present, many new transsexual men are being started on subcutaneous Testosterone Cypionate injections instead of IM in the Northern California area. Is it possible I played a role in this? I’ve used my contacts with local hormone expert Jennifer Hastings MD and indirectly through many patients in the area — but who knows. But as of today, in California, transsexual women still need to boldly request subcutaneous administration from their doctors, who may never have had clinical experience with it. This situation has been improving rapidly throughout 2017 and we can expect that to accelerate as news of the Mayo Clinic program spreads. In the meantime, subcutaneous hormone administration has also became accepted in one Canadian province with good results, according to another report.
Recently, Fenway Health in Boston has begun advising subcutaneous injection of hormones for trans people, and including a detailed procedure in their handout. (4) However, they advise using an 18g needle for drawing from vials, which may cause damage to the seal to accumulate faster than necessary. I use a 22g needle for drawing. They also mention a 5/8ths inch needle, 25g or 26g, instead of the 1/2 inch 30g needle I suggested above. The 30g will generally cause significantly less injection pain.
Informal group knowledge, consisting of around 50 subcutaneous Estradiol-using trans women, seems to favor using subcutaneous over IM. The users cite the advantages of comfort and ease, and often express relief that they don’t have to wrestle with awkward positions to give themselves proper buttocks IM injections. Patients who had been using thigh injections (which give poor bioavailabililty and halflife compared to buttocks IM) may report some improved feminization effectiveness and improved mood and emotional stability. SubCut injections may also make it easier to go from a long cycle (7 day) injection schedule to a shorter one (twice a week). A few users have complained of stinging — but this may be due to not allowing alcohol to dry adequately, or not using proper needles.
With modern knowledge that parenteral estradiol has major health benefits over oral estradiol, there was still a missing piece of the puzzle: a convenient and safe personal injection method. It’s clear that subcutaneous injection of oil-based hormones is in many ways, an important step forward in establishing injection as the most favored administration method for oil-based sex hormones.
============================================================
(1) “Comparative pharmacokinetics and pharmacodynamics after subcutaneous and intramuscular administration of medroxyprogesterone acetate (25 mg) and estradiol cypionate (5 mg).” Contraception. 2011 Dec;84(6):565-70. doi: 10.1016/j.contraception.2011.03.014. Epub 2011 May 11.
(2) Callie Amber Foxx, private communication, Nov. 2, 2017.
(3) “Subcutaneous Injection of Testosterone Is an Effective and Preferred Alternative to Intramuscular Injection: Demonstration in Female-to-Male Transgender Patients”, Spratt, The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 7, 1 July 2017, Pages 2349–2355, https://doi.org/10.1210/jc.2017-00359
(4) “Transgender Health Injection Guide” no visible date, Fenway Health, Boston MA. [link]
This post is so timely for me, thank you. I started HRT on pills two months ago and a friend strongly suggested that injections are the best for multiple reasons. I’m scared, of course, and yet the subcutaneous approach sounds like something I could do. I’ve sent my doctor a link to this so we can talk about it on Wednesday.
Thank you!
LikeLike
Good luck Emma! Getting the right syringes and needles is very important — please don’t let your doctor or pharmacist push you around in that respect. Very few medical professionals seem to know the ideal way to inject oily hormones subcutaneously. The links in the article above are the best ones I know of right now, and I’ll continue to add to them.
LikeLike
[…] needed, from Walgreens, plus about $0.35 in cost for syringe and needles per injection. See the subcutaneous article for details on injection […]
LikeLike
[…] showed that 61% were using gluteus injections, 28% using thigh, and 11% using subcutaneous. See our article for more details on the preferred equipment and the patient experience. Group experience reports an […]
LikeLike
Thank you so much for posting this. I’ve been doing IM injections in my thighs alternating with each round of injections. Your comment that some M to F may skip or prolong the time between doses due to the discomfort of IM injections hit home for me. I have gotten to where I dread them.
I’ll definitely speak with my MD at my next appointment about sub cu injections,
LikeLike
I watched a few of your videos on injections. I noticed in one you did not do a separate plunge needle, then switch to an injection needle; You went straight from the vial to your abdomen, and I was wondering why. Thank you.
LikeLiked by 1 person
In that one, the needle was not removable from the syringe. It was a one piece, with a 30g 1/2 inch needle on a 0.3ml syringe. It’s convenient to draw with the same needle you inject with, and safe, but the needle can get slightly duller when it pierces the seal, making the injection less comfortable. But if you are careful with where you pierce the seal, you can avoid dulling the needle. The other disadvantage is that the needle is a bit slow drawing up, but who’s in a hurry?
LikeLiked by 1 person
I do agree with all of the ideas you have presented for your post. They are very convincing and will definitely work. Nonetheless, the posts are very brief for newbies. Could you please lengthen them a little from subsequent time? Thanks for the post.
LikeLiked by 1 person
[…] assume you are on a nearly-ideal regimen of injected Estradiol Valerate, 5mg twice a week, subcutaneously. (Once a week regimens are a little less effective.) Have your physician write a prescription for […]
LikeLiked by 1 person
“… you MAY choose to use the all-in-one insulin syringe.”
Have you tried this? Because it clearly doesn’t work!!!
My levels have pretty much dropped to zero now.
LikeLike
What do you mean it doesn’t work?
LikeLike
I ended up figuring it out.
The needle is too short, so every now and then I’ll end up doing a subdermal injection. Hormones will get stuck in the skin, leaving a painful noticeable lump for well over a week (or 2). Also, there will be a lot more pain and resistance while pushing the plunger down and a lot will leak out afterward.
So what I ended up doing is this:
Inject in the thigh instead. No risk of going too deep here, and it’ll hurt less afterwards.
Don’t bother bunching up the skin, it’ll just increase the risk of going subdermal. I do a z-track instead.
Jab the needle straight in, and press the syringe firmly, denting the skin.
Push the plunger down, there should be no resistance. If there is, then I didn’t go deep enough.
Uptake should be rather fast, usually I notice it within half a day.
LikeLike
Assuming that even many post -op transwomen use estradiol valerate, is it possible for a pharmacy to compound 10mg/mL in an aqueous suspension so that it could be delivered subcutaneously? That would allow me to use Owen Mumford’s Autoject 2 pen-inexpensive, reusable and essentially painless, say many Amazon reviews. Plus a 10mg dose would mean that I’d only have to stick myself once every seven days, not every day, if subcutaneously deliverable estradiol is only possible at 1mg/mL. Is it only a matter of finding the right pharmacy, or am I asking for the impossible? Please advise ASAP. Thanks.
LikeLike
The subcutaneous technique for hormones in oil is described in this article. I don’t think the aqueous solution you describe would be practical. If a painless solution is your object, then the key is using the right needle and syringe, as described above.
LikeLiked by 1 person
Based partly on your reply my endocrinologist then suggested that I switch from the 20mg/0.5ml of estradiol valerate once every 14 days that I’ve been using forever to 1.5mg/1ml of aqueous estradiol daily. Would this be the ideal approach if daily injections would virtually guarantee constant levels and (hopefully) improve and maintain bodily changes (hair)?
However, if it were not for this particular autoinjector I could never bring myself to self-inject.
https://www.adwdiabetes.com/product/4473/owen-mumford-autoject-2-fixed-needle
Unfortunately for me I have to accept a tradeoff, where in order to have access to a subcutaneous autoinjector for sale in the US it has to work with aqueous only drugs. And
I believe that the OM Autoject2 is the only fully automatic model, but which can’t inject oil based estradiol subcutaneously-which presumably would yield a longer estradiol half life, as the compatible needle is too short and thin. Thus, I have to inject daily.
https://www.owenmumford.com/us/patients-product/autoject-2/
However, assuming all the while that a shorter and thinner needle would less painful I just bumped into this https://www.indiatoday.in/magazine/living/story/20001120-bigger-thicker-needles-hurt-less-than-smaller-thinner-ones-study-778784-2000-11-20
But if I inject in my stomach lying down could I still expect little pain if the AutoJect2 pen is loaded with this compatible syringe?
https://www.adwdiabetes.com/product/1279/bd-ultra-fine-u100-syringes-31g-3-10cc-5-16in-90ct
Please advise
LikeLike
On another matter, while I haven’t yet verified this with my endocrinologist or the compounding pharmacy, I assume that they made bioidentical rather than synthetic aqueous estradiol for me. I’ve been using synthetic estradiol valerate for > 20 years (Steris Labs, Squibb, Sandoz, Perrigo, et al). Ironically, I have heard conflicting reports on the safely of
using bioidentical rather than synthetic hormones. Any cause for concern?
LikeLike
Being synthetic does not prevent estradiol valerate from being bioidentical. In the body it separates into real human-identical estradiol plus a harmless valerate ion.
LikeLike
The research paper you reference was authored primarily by my Endo (Daniel I Spratt, MD). He has had me on SubC injections of Delestrogen (Estrodiol Vallerate for 3 years now.). I’m extremely satisfied with it (over the pill version). He prescribes an injection once a week, but recently I have noticed a psychological dip in my emotions at about the 5th, 6th or 7th day. I’m going to start with your twice a week recommendation immediately. As an aside, I would be interested in any reputable recommendations for estrodiol levels for a MTF in her 60s. I am not contention with my endo’s recommendation that my estrodiol levels approximate those of a post menopausal women. Our bodies, after all are different, our medical histories are different, and I see no need for an equivalency of hormone levels.
LikeLike
I was wondering, my doctor wants to inject me in the stomach for my SubQ. This will be my first shot fellow sublingual. This isn’t beneficial is it in your opinion? We need it in the buttocks?
LikeLike
‘following
LikeLike
I tried to post earlier that thi si the way I have been doing it, but injecting weekly. Have you tried it? Does your doctor want you to inject once or twice weekly?
LikeLike
This is the way I have been doing it. I much prefer it over IM. However, I am here to learn more and to evaluate whether I should let my doctor switch me to patches.
LikeLike
My First Year With Estradiol Aqueous
It’s been a year this month since my endo at Winthrop Hospital here on Long Island-mostly based on his own research and perhaps partly on what’s been discussed at this and other trans community forums-suggested that I switch from 0.5 mg of 40mg/ml estradiol valerate every 14 days (which I’ve used for > 20 years) to 0.73cc of 1.5mg/ml estradiol aqueous daily, which a local pharmacy compounds for me.
YMMV, but in my case I found estradiol aqueous seemed to improve breast shape and texture. But I was especially overjoyed to find the thickness, density and texture of my hair had improved quite substantially. Presumably, the latter benefit happens because daily rather than once bi-weekly injections keep my estrogen levels virtually constant.
However, I cannot overemphasize the need to maintain a highly nutritious diet-plenty of large, fresh green salads (dark green romaine or spinach leaves, red pepper, cumber, carrots, red onion). I alternate salads with steamed broccoli/peas/carrots. Lots of fresh fruit (org strawberries, red grapes, org apples). Don’t forget a quality protein two to 3x daily; not too much or too little. Replace conventional sweets with air popped corn, oatmeal (I like it with some blackstrap molasses) or toasted multi grain with smears of org blue, straw or raspberry preserve.
Listening to your body helps with regulating everything you eat and do to it!
Plus at least 45 minutes of exercise every other day is a must! Until COVID 19 hit I had access to my co-op village’s excellent gym; great programmable treadmills and bikes and a “Tough Stuff” weight machine. With all gyms closed throughout New York state, I walk 1.5 miles roundtrip @ ~ 2 mpg every other day. And I use a pair of 6.6 lb free weights at home. I miss the gym machines like crazy but they may not be available until there’s a COVID vaccine, so we may have to stick with these and other machineless exercises.
The compounded 10% minoxidil + Betamethasone topical my dermatologist prescribed has certainly helped, but I’d estimate the estradiol aqueous has improved my hair by at least another 35%.
Last but not least, what’s also exceptionally wonderful about switching to aqueous estradiol is that for the first time I can now do my own injections. Though self-injecting anything from insulin, to hormones and more is essentially commonplace, I have always been “psychologically” unable to do so manually. Consequently, this cost me many
long years in commuting and doctor visit copays. But unlike estradiol valerate, estradiol aqueous can be delivered quickly, easily and all but completely pain free via an inexpensive and reusable Owen Mumford fixed needle autoinjector and BD Ultrafine syringes, albeit this insulin autoinjector used off label.
Autoinjecting also gave me a big shot of self-respect and independence as I can now take care of this ridiculously simple chore all by myself.
Autoinjecting still doesn’t exactly make sticking myself a fun thing, and years of losses incurred to get bi-weekly injections will always been lamentable. But I can take comfort in discovering estradiol aqueous, where for the most part my health and appearance has since never been better. Again, YMMV, of course.
LikeLike
I’m interested in how you managed to get a US compounding pharmacy to mix this up for you. This is not a conventional prescription in the US anymore, though perhaps it was used in the 50’s and 60’s still. Can you state how the prescription was written?
LikeLike
Hi Beverly!
So I’ve been on HRT for 8 years now, and I’ve never once gotten down to female levels (at least, according to blood tests). Spiro has had *nasty* but subtle side effects for me, so I’m only now getting off of it, and while I was on EV injections for a year they never seemed super effective – though I was doing them intramuscularly in my thigh, which is apparently not the ideal location. I wanted to check in to confirm how I should actually be doing the injection, since I’m back on them now.
The instructions on my bottle of EV (40mg/mL strength) say ‘Inject 40mg (1mL) intramuscularly every 10 days’. So according to this, I should instead be doing ‘Inject 20mg (0.5mL) subcutaneously every 5 days’? That would put the dosage at 0.5cc, which means that I would be using Case #1 above and all of the listed supplies. Then I would draw/inject 0.5mL of the fluid four inches from my bellybutton (putting it at about halfway between my hip and said navel), putting the needle straight in while I do it, and repeating that every five days at alternating sites. Is that all correct?
Finally, one of my friends said that subcutaneous injections of the wrong medications can cause a lot of issues, but can I assume that that’s not the case here? There’s also that comment above about the needle (of the 0.3cc insulin syringes) not getting deep enough and it getting injected into the skin instead, but that shouldn’t be an issue for the needles I’m going to be using, right?
Sorry for the long comment, but I tend to be a worrywart and I’m anxious about going ‘off the book’. But I’m also tired of doctors not knowing what to do and my levels being stuck this high, so I’m willing to take things into my own hands this time around 😛 Plus, subcutaneous injections just sound easier overall.
Thank you for your reply!
LikeLike
Hi Beverly,
In reply to your post 5/30/20, t says on the 28mL vial: 1.5mg/mL once daily. I use 70 units daily. But why did you say that using estradiol aqueous is not “practical”? It is because it makes it harder to control my weight? Thanks to COVID all the gyms have been closed for months-including of course the one in the co-op village I where I live. So I briskly walk over a mile every other day, do free weights and do 100 push ups against the wall. I never drink any alcohol (always made me depressed as well as fat) and eat no sugar. 10 minutes each on programmable high intensity interval bikes, treadmills and weight machines 4 to 5 days weekly did the trick before COVID but now I’m so fat that I have wear stretch pants on the job.
Today I decided to try injecting only every other day for a week or two and see if I feel and look okay. If yes, hopefully I will lose some weight in the process. If start to feel achy and/or if my hair texture changes or starts falling a lot then maybe change to every third day, al least until (IF??) gyms open again. Except for this disastrous weight gain, estradiol aqueous has clearly improved my hair. I’ve almost completely regained my hairline and there’s been substantial regrowth over much of the scalp. Of course, along side of this I do lots of other things for my hair: Carefully applied but thorough daily “squeezing” scalp massages prior to applying 10% minoxidil + Betamethasone, oral minoxidil + aldactone, basic supplements including daily RDA doses of potassium citrate. And I just added the HairMax laser. Welcoming any shared facts and suggestions.
Sent: Wednesday, July 29, 2020 at 11:00 PM
LikeLike
[…] long needle, and do the injection shallowly at an angle into the fatty layer of the abdomen. See my main article on this subject. Because the needle is very thin, the pain level is very low, but as with the LIM […]
LikeLike
Thank you Beverly for sharing all this helpful information. I’m about to make the switch from IM to subQ, and hope I can “come back” to the BD 1ml syringes, but I’m curious about your thoughts about something: It has been completely impossible for me to inject EV 20mg/ml in any quantity through a 25ga 1-inch needle and BD 1ml syringe. I’ve had to use the Monoject 3ml, which has twice the diameter and is softer than the BD 1ml. Why do you suppose that should be? It makes no sense to me. I would have thought syringe cross-sectional area would be directly proportional to injection force, but I just can’t seem to depress the plunger with the BD 1ml, and it worries me that it might be even worse if I go subQ with a 30ga needle albeit mitigated at half the length. Thanks again!
LikeLike
[…] quadrant of the buttocks. For subcutaneous injections, put on a 0.5 inch 30g needle, instead, and follow these instructions for a shallow injection into fat around the abdomen or […]
LikeLike
hi, considering the SubQ you use a 12mm needle inyecting at 45-ish angle, wouldnt that allow us to use a shorter needle (8mm) but inyecting at a 90 degree angle?
LikeLike
There may be advantages to having the longer needle path through fatty tissue, to prevent movement of the bolus upwards towards the dermis, where the hormones would be more rapidly absorbed by the system and lost. I would suggest going the opposite way, even, with a 15mm needle at a 30 degree angle.
LikeLike